Joint Pain Causes & Treatment Options
Don’t Let Joint Pain Slow You Down
From walking to bending, turning to jumping, your joints are what keep you moving in nearly every activity. When all is functioning as it’s supposed to, your joints allow movement without hiccups and without pain. But when a joint becomes diseased or damaged, whether from a specific incident or oncoming arthritis, pain is almost guaranteed to get in the way of regular daily movements.
It’s so important to understand the causes of orthopedic joint pain and treatment options. And more importantly, it’s important that you have hope of one day getting back to the activities you love, but without the joint pain that has been holding you back. Whether you are curious about your eligibility for total joint replacement surgery or about the many other available joint pain treatment options, this website is here as a helpful resource for you in your journey to achieving relief from your joint pain.
Gaining a solid understanding of the different procedures available for joint pain relief will help you choose the best course of treatment. Once you’ve read through the available resources on the Joint Team website, do not hesitate to ask your orthopedic doctor in Fort Myers, Estero and Naples any questions you may have.
Understanding the Causes of Joint Pain
What is a Joint?
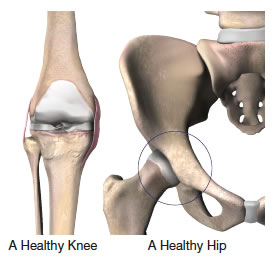
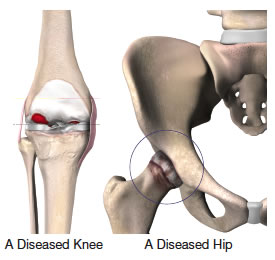
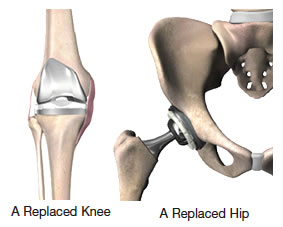
In short, a joint is a part of the body where two or more bones meet to allow movement. Connected by thick bands of tissues called ligaments, joints can take on many different shapes and forms. Examples include the knee joint which is formed by the lower leg bone (tibia or shin bone) and the thigh bone (femur). The hip joint forms a ball-and-socket connection, with the femoral head acting as the ball at the top of the thigh bone closest to the hip, and the acetabulum in the pelvis acting as the rounded socket.
Covering the ends of the joint bones is a smooth, soft, yet incredibly strong material called cartilage that creates a low friction environment for the bones of the joint to move against each other. Where cartilage does not coat the joint’s surface, a soft lining called synovium does. It is essentially a type of tissue that produces synovial fluid that lubricates the cartilage and bones inside the joint capsule.
Common Causes of Joint Pain
One of the most common causes of joint pain is arthritis, effecting over 20% of adults in the United States. Types of arthritis include:
Osteoarthritis (OA)
Because it involves the breaking down of cartilage and synovial tissue, osteoarthritis is sometimes called degenerative arthritis. The bones begin to press against each other during movement, causing pain and stiffness as the joint’s protective surfaces wear away. This form of arthritis is usually found in adults over the age of 50 and in families with a history of osteoarthritis.
Rheumatoid Arthritis (RA)
Rheumatoid arthritis, the most common type of autoimmune arthritis, causes chemical changes in the synovium fluid that causes your body to inflame healthy tissue, destroying cartilage and causing pain and swelling. This type of arthritis affects women about three times more frequently than men, and if left untreated can cause permanent damage to the joint.
Post-traumatic Arthritis
Post-traumatic Arthritis is caused by the wearing out of a joint that has been damaged from any physical injury, whether from sports, a fall, or an automobile accident. This type of osteoarthritis will usually develop in an injured joint where the bones and cartilage have not been properly tended to. When the surface of the joint is no longer smooth as a result of the injury, further damage will occur, worsening the problem.
Avascular Necrosis
This type of arthritis, also known as osteonecrosis, can develop when there is a shortage of nutrients from blood being delivered to a bone’s cells. As a result of this disrupted blood supply, the bone’s structure and the cartilage covering it will weaken and could eventually collapse. There is research that suggests that prolonged use of corticosteroid medicines can lead to avascular, along with diseases like Chrohn’s, excessive alcohol intake, and injuries.
Obtaining a Quality Diagnosis
In the case that the treatment you have received by a family doctor, internist, or rheumatologist has not provided you with relief from your joint pain, you may want to consider consulting an orthopaedic surgeon to discuss whether surgery is a viable option. It’s possible that upon meeting with an orthopaedic surgeon you will be given an arthritis diagnosis for the first time.
The Orthopaedic Evaluation
Although the process of an orthopaedic evaluation varies from doctor to doctor, there are several common tests that you should expect to see when being examined by an orthopaedic surgeon. The evaluation will likely involve:
- A thorough medical history
- A physical examination
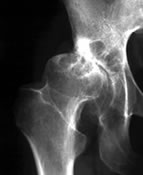
- X-rays
- Additional tests, as needed
Your medical history is taken into account when being evaluated for joint replacement surgery. In addition to your medical history, everything from your posture to your way of walking will help to narrow down the possible causes of your joint pain. This examination will also allow the orthopaedic surgery to assess other important details of your jointed areas, such as:
- Size and length
- Strength
- Range of motion
- Swelling
- Reflexes
- Skin condition
Your back may be examined during your evaluation if you suffer from pain in your hip, as it may be caused by issues in your lower spine.
X-ray evaluation will usually be the following course of action in providing an accurate diagnosis. X-rays help to show the severity of the joint damage or any deformities such as:
- Decreasing space between the joints
- Cysts in the bone
- Spurs on the edge of the bone
- Areas of bony thickening called sclerosis
- Abnormal or incorrect alignment
Additional tests like blood, urine, or joint fluid samples may be needed to confirm a specific arthritis diagnosis and rule out other diseases. Certain types of X-rays focusing on the spine can contribute to ruling out any back problems as the source of hip pain. Magnetic Resonance Imaging (MRI) or a bone scan may also be used to evaluate the current state of your bones and soft tissues in the joint being examined.
- To help the orthopaedic surgeon in making an accurate diagnosis, it would be wise of you to record answers to the following questions before your evaluation: Where and when do I have pain?
- How long have I had this pain?
- Do I have any redness or swelling around my joints?
- What daily tasks are hard to do now?
- Did I ever hurt the joint or overuse it?
- Does anyone in my family have similar problems?
Joint Pain Treatment Options
The orthopaedic surgeon will consult you about the results of your evaluation and discuss your surgical and non-surgical treatment options based on the diagnosis provided, possibly involving:
- Medication
- Physical therapy
- Joint fluid supplements
- Joint replacement
Medication
One of the many different types of medications commonly prescribed to treat symptoms of arthritis is non-steroidal anti-inflammatory agents, or NSAIDs. These drugs can be taken for long periods of time in order to reduce both the discomfort and inflammation that comes with arthritis.
Corticosteroid injections may also be prescribed to help combat swelling and offer rapid pain relief. On the flip side, unlike NSAIDs, corticosteroids can only be used a couple times a year because they are known to cause bone and cartilage to weaken over time, and can potentially cause other serious side effects. For this reason it’s extremely important that their use and effects are closely examined by a physician.
Physical Therapy
In treating the various forms of arthritis, a physical therapist may recommend Isometric (“pushing”) exercises to help strengthen muscles without causing further wear on inflamed joints, and Isotonic (“pulling”) exercises to strengthen muscles and help maintain their longevity. Daily movements like gentle walking with a cane or other assistive device will also greatly help with recovery.
Joint Fluid Supplements
A patient’s knee can be injected with a joint fluid supplement that essentially acts as “joint grease” if they do not find relief with other joint pain treatments. This lubricating injection may offer temporary relief, with varying results from patient to patient. Joint fluid supplements are not cures for a diseased knee, and a patient may want to consider a total joint replacement surgery if pain intensifies over time.
Total Joint Replacement
While circumstances may vary, patients suffering from severe arthritic symptoms are generally recommended total joint replacement surgery if:
- Ordinary daily activities are restricted by functional limitations of the affected joint.
- Other treatments like those mentioned above, the use of an assistive device, and restricting certain activities do not relieve pain.
- There is intense stiffness in the joint.
- X-rays suggest the development of advanced arthritis or other issues.
What is Total Joint Replacement?
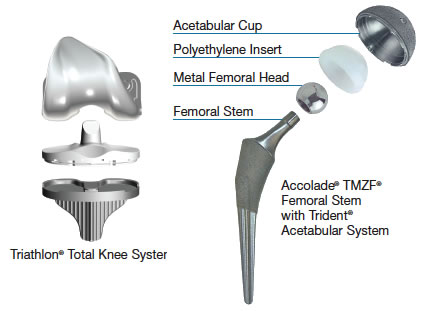
During a total joint replacement surgical procedure, components of an arthritic or damaged joint are carefully taken out, and a plastic or metal device called a prosthesis is put in its place. The prosthesis’s purpose is to allow for natural movement in the way that a natural joint would.
In a hip replacement procedure, the femur (head of the thigh bone) and acetabulum (hip socket) is typically replaced with durable metal and a plastic called polyethylene, respectively. In total knee replacement, the top of the femur (thigh bone) and top of the tibia (shin bone) are resurfaced with similar materials. The prosthesis is then attached using either bone cement or a material that will allow bone tissue to grow into it.
Since the 1960s, total joint replacements of the hip and knee have been performed with increasing success in restoring function and reducing pain. Today, 90% to 95% of patients are able to return to their normal activities with reduced pain after a joint replacement procedure.
Although it’s difficult to estimate the lifespan of joint replacements, today’s patients can potentially undergo procedures that utilize new advances in technology that could increase the lifespan of the prostheses.
Recent Advances in Total Joint Replacement
As successful as most of the approximately one million annual hip and knee replacements performed in the U.S. are, artificial joints sometimes loose their strength over time, requiring a revision (repeat) surgery.
The issue of artificial joint devices weakening over time – along with the facts that an increasing number of younger and more active patients are undergoing a joint replacement procedure and older patients are living longer – has presented a real challenge to the medical field to try and increase the lifespan of the prosthesis used during replacement surgeries.
The increasing availability of materials such as titanium and ceramic along with improvements in surgical techniques and instrumentation provides orthopaedic surgeons with promising alternatives to conventional materials that may help increase the lifespan of a joint replacement procedure.
Avoiding Complications After Joint Surgery
Serious complications following a joint replacement surgery such as an infection occur in less than 2% of patients. Although this is very low, it’s always important to familiarize yourself with the complications that could arise from a total joint replacement or any surgical procedure for that matter. Most of these complications can be successfully avoided and/or treated.
Infection
An infection can develop in the surgical scar or around the area of the affected joint either in the hospital, after the patient is released, or possibly even years after the surgery. Following a total joint replacement surgery, patients will be given antibiotics to help avoid infection and, in some cases, may need to take antibiotics before undergoing even small medical procedures in the future as to lessen the risk of an infection spreading to the new joint.
Blood Clots
The decreased mobility of a patient following surgery and subsequent slowing of blood movement throughout the body is one of the more common ways that blood clots can develop. Some methods of reducing the risk of post-operation blood clots include:
- Blood thinning medications (anticoagulants)
- Elastic support stockings that improve blood circulation
- Plastic boots that inflate with air to promote blood flow
- Elevating the feet and legs to keep blood from pooling
- Regular walking and gentle movements
Lung Congestion
Patients are assigned a series of deep breathing exercises to decrease congestion in the lungs as a way of combating the risk of pneumonia following a total joint replacement surgery.
Getting Moving Again
You may be surprised to learn that patients are encouraged to get up and start moving around as early as the day of your total joint replacement surgery.
As soon as it is safe for you to do so, you will be recommended several exercises that target the new joint in order to speed up your recovery. Pain medication may be recommended prior to physical therapy to ease the inevitable stiffness and soreness. Along with these exercises, a physical therapist will also provide you with additional plans for rehabilitation after your discharge from the hospital.
Regular activities such getting dressed, bathing, and grabbing items off of shelves may require the help of certain devices which an occupational therapist will provide instruction on how to use. A case manager will help to prepare you for your return and make sure that you have plenty of support in place for a speedy and safe recovery.
Life Following Your Total Joint Replacement
Although joint replacement surgery will provide most patients with significantly reduced joint pain and improved ability to participate in the activities of daily living, it won’t provide patients with newfound strength that they never had before. It’s important to listen to your doctor’s recommendation regarding the appropriate level of activity you should be taking part in.
You can expect certain limitations to be placed on your activities after a total joint replacement surgery. This may include having to use a can or walker, or refraining from jumping, kneeling, and bending. It could take six weeks or so before you can begin driving, so be sure to ask your orthopaedic surgeon and physical therapist about your specific limitations.
While most patients can get back to their jobs once fully recovered, those in certain industries – such as construction, carpentry, or other occupations that involve repeated high climbing – may be advised to refrain from the physical aspects of these jobs. In addition, certain strenuous athletic activities such as basketball, skiing, distance running, or contact sports should be avoided.
Keep in mind that acceptable physical activities after a total joint replacement procedure should:
- Not cause immediate pain, or pain felt later
- Not jar the joint, as will occur with running or jumping
- Not push the joint to the extremes of its range of motion
- Be overall pleasurable
Joint pain and damage will increase with weight gain, so it is important for an individual with an artificial joint to maintain a normal body weight.
Talk to Your Doctor
If medication and other conservative treatments for your joint pain have not provided you with sufficient results, it may be time to consider a total joint replacement surgery in Fort Myers, Estero and Naples. It’s a good idea to bring up any and all questions and concerns and with your doctor, but just be sure to make notes of his or her recommendations.
Remember that even if your doctor determines that a total joint replacement is a viable course of action for you, it is still your choice to undergo the procedure. Always explore your treatment options so you can one day return to the activities you love and achieve the relief you long for.
To learn more about Joint Pain treatment options in the Fort Myers, Estero and Naples area, contact Orthopedic Center of Florida.
References:
1. Arthritis Foundation website, accessed February 2009.
2. American Academy of Orthopaedic Surgeons website, accessed January 2009.
3. American Academy of Orthopaedic Surgeons website, accessed January 2009.
4. Hanssen, A.D., et al., “Evaluation and Treatment of Infection at the Site of a Total Hip or Knee Arthroplasty,” JBJS, Volume. 80-A, No. 6, June 1998, pp. 910-922.

